This resource will be continuously updated as evidence and guidelines emerge. Information was correct at time of publishing. Date Updated: 22/11/2022
What is Long COVID?
What is Long COVID
As COVID-19 is a new disease, research and evidence-based guidelines are constantly evolving to ensure best management of this disease. Most people who experience COVID-19 will have symptoms that resolve within approximately 12 weeks.
However, for some people their symptoms may persist or worsen, and they continue to experience symptoms or develop new symptoms as described in the Ongoing (4-12 weeks) and Post COVID-19 Syndrome (12 weeks onwards) stages of COVID-19. An umbrella term called Long COVID is used to describe the cluster of signs and symptoms that people continue to experience or develop after acute COVID-19.
Patients will describe symptoms that persist and fluctuate getting better or worse but overall have an effect on their quality of life and can affect many systems in the body.
There is currently no link between severity of initial COVID-19 infection and the long-term effects of COVID-19 on an individual.
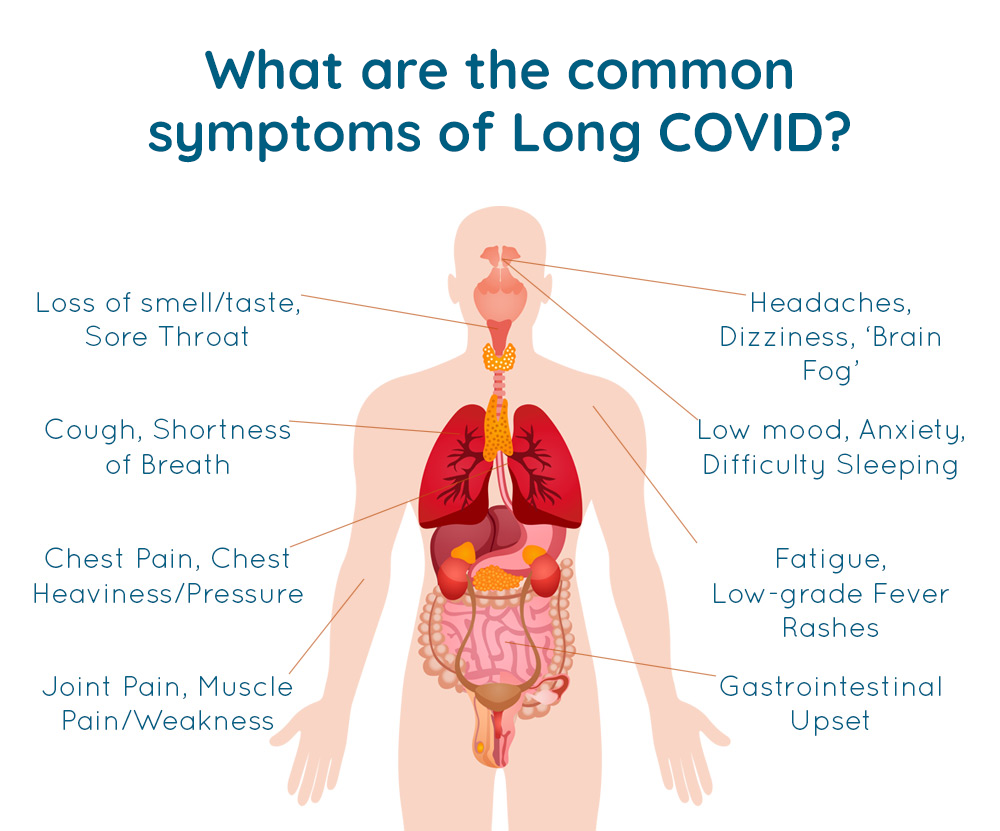
What are the symptoms?
Long COVID may affect many systems in the body and can include fatigue, dry and irritable cough, shortness of breath and breathlessness or heart, lung, kidney, neurological or musculoskeletal issues.
Examples of Symptoms: * source https://elearning.rcgp.org.uk
- Fatigue
- Shortness of Breath (Dyspnoea)
- Headaches, Confusion or Seizures
- Reduced concentration or “brain fog”
- Joint or muscle Pain
- Chest Pain or tightness
- Cough
- Loss of Smell (Anosmia)
These symptoms can impact on psychological features following COVID-19 and include:
- Sleep Disorders
- Trauma Disorders
- Impaired Concentration
- Fatigue
- Impaired memory
Fatigue
Fatigue is a feeling of extreme exhaustion and is the most common symptom of Long COVID. It:
- is not easily relieved by rest or sleep
- is not the result of unusually difficult activity
- can limit functioning in day-to-day activities
- negatively impacts quality of life
Post Exertional Symptom Exacerbation (PESE)
PESE is a disabling and often delayed exhaustion disproportionate to the effort made. They are sometimes described as a “crash”. The activity that can trigger this worsening of symptoms can be something that was easily tolerated before, such as:
- a daily activity (eg a shower)
- a social activity
- walking (or other exercise)
- reading, writing or working at a desk
- an emotionally charged conversation
- being in a sensory environment (eg loud music or flashing lights)
PESE is most often triggered by physical activity and exercise. Nearly 75% of people living with Long COVID still experience PESE after 6 months.
The symptoms worsened by exertion can include:
- disabling fatigue/exhaustion
- cognitive dysfunction or “brain fog”
- pain
- breathlessness
- heart palpitations
- fever
- sleep-disturbance
- exercise intolerance
Symptoms typically worsen 12 to 48 hours after activity and can last for days, weeks or even months.
If you think you have PESE, what can you do to help self-manage it?
Regardless of you experiencing PESE or not, a symptom diary is a really useful way to keep a daily track of how you are feeling. Track your symptoms – duration, what potentially triggers them, what improves them and how you are progressing with each day, week, and month.
Remember that symptoms can be not only triggered by physical exertion but cognitive, mental and emotional exertion also.
Once you begin to discover when your symptoms occur and what potentially both triggers and improves them. You can then start to manage them with the guidance of your physiotherapist.
Click here to access sample symptom logs
If you are not experiencing PESE, recovering and self-managing well?
If you were not hospitalised from COVID-19 and are recovering at home and not experiencing PESE or any Long COVID symptoms (4-12 weeks onwards). Then you can safely begin to increase your physical activity and formal exercise levels. The WHO have more advice here. If you were to experience any of the above, please stop the activity immediately and seek medical assessment.
- new onset of shortness of breath or chest pain, palpitations or chest tightness or a sensation of pressure in your chest
- reduced blood pressure or dizziness
- increased fatigue during or after the activity
- if you have been given a pulse oximeter ensure oxygen levels are above 93%
How to use pacing with your physiotherapist
Pacing is a self-management strategy during activity to avoid PESE. When pacing you do less activity than you have energy for, keeping activities short, and resting often.
1. Learn about your energy reserve/reservoir
- Your energy reserve is how much energy you have each day – this will vary so it is best to find your baseline by using an activity and symptom diary. Your “baseline” is what you can do fairly easily on a good day and only just do on a bad day.
- You should always aim to leave some energy at the end of the activity or day– don’t keep going until you feel tired.
2. Learn how much energy you have
Your activity and symptom diary should start to show some patterns. You can now reduce or modify your activity levels so that you don’t trigger PESE or “crash”. This will help you find a level of activity you can maintain on both good and bad days, unless you have a relapse. Learn to recognise early signs of PESE and immediately initiate stop, rest, pace to avoid a crash.
3. Learn how to use the 4 Ps to help you plan your activities
- Prioritise what you really need to do in a day or week. Question whether all activities are necessary. Can someone else do it? Can I change the activity so it is easier for me?
- Plan in your main prioritised tasks for the day. Plan in your rest time so the day is paced.
- Pacing – break up your activity into smaller, more manageable tasks with rest breaks.
- Pleasure – spend some energy on things you enjoy to help improve your quality of life.
4. Learn how to save energy
- Learn to say no.
- Modify your activities to use less energy.
- Avoid the temptation to “do just a little more”.
- Take short cuts and ask for help.
5. Learn to rest between activities
- Rest means absolutely minimal activity and little or no mental stimulation.
- During rests avoid activities that can be stimulating, such as TV and social media.
- Try some meditation and/or breathing exercises instead.
Can I ever do more?
- When your symptoms improve you will experience less weakness and fatigue. Work with your physiotherapist to find out how to increase your activity levels very gradually, such as carrying out some core strengthening exercise or increasing the amount you can walk by 10%.
- Be realistic and stay flexible – try to create a weekly routine, but accept that some days you will need more rest than others and avoid your triggers.
- Focus on your accomplishments instead of symptoms or what you have not achieved.
GUIDE
Post COVID-19 Rehabilitation Guide
This guide is designed to give you simple advice to help you recover from COVID-19.